Healthcare worker Q/A
To get more information about what working in healthcare is like during a pandemic, we interviewed three medical workers in the ISD Community who are currently experiencing changes in their workplaces.
May 23, 2020
Where do you work, and what do you do there?
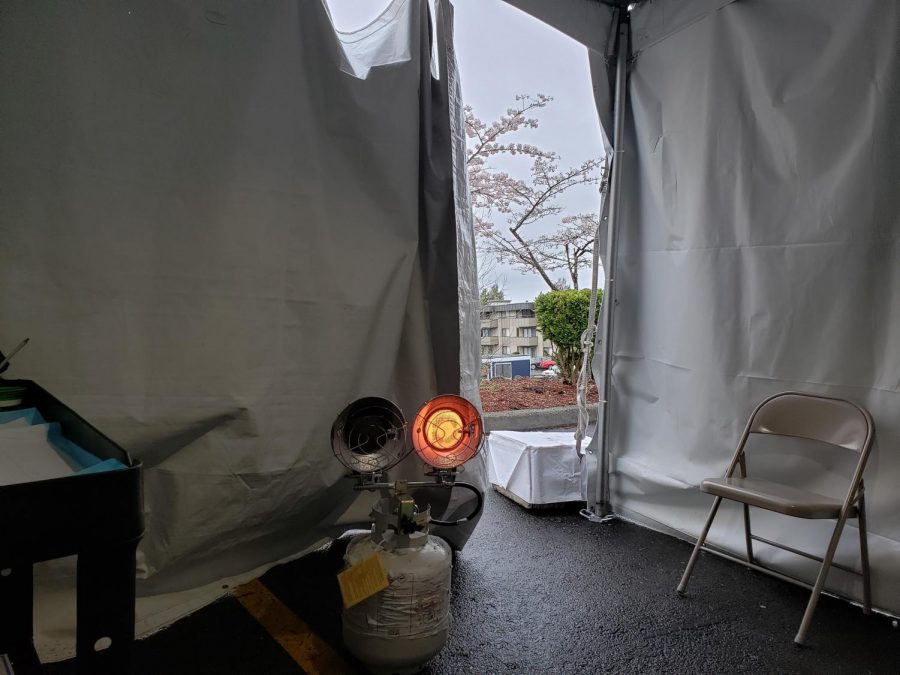
Chantel Turner: I work at Valley Medical Center in Renton. Normally I am a physician assistant working in the otolaryngology (ear, nose, and throat) / head and neck surgery clinic. Since the COVID pandemic, I have been volunteering in what are known as ” URI Screening Tents”, where we screen people who are sick with possible COVID symptoms.
 Marianne Kampf: I work at Sound Mental Health, a community-based facility, which offers counseling, medication treatment, substance use disorders for people with a variety of mental health illnesses, and addictions. I’m a Psychiatric Nurse Practitioner and work with people who suffer from substance abuse and mental illness. I assess, diagnose, and treat people, provide daily medication management, and referrals to other health care providers and interact with clients’ medical providers. I also provide consultation to clinicians and other healthcare workers.
Marianne Kampf: I work at Sound Mental Health, a community-based facility, which offers counseling, medication treatment, substance use disorders for people with a variety of mental health illnesses, and addictions. I’m a Psychiatric Nurse Practitioner and work with people who suffer from substance abuse and mental illness. I assess, diagnose, and treat people, provide daily medication management, and referrals to other health care providers and interact with clients’ medical providers. I also provide consultation to clinicians and other healthcare workers.
Brianna Sherwood: I work at Franciscan Heart and Vascular in Tacoma, WA. We have a total of 15 cardiologists which are divided into General Cardiology, Heart Failure, and Electrophysiology. I work closely with our general cardiologists to help our patients maintain good cardiac health. Our daily tasks can include: triaging patients as they call into the clinic, calling patients about results, placing heart monitors, running treadmill exercise tests, running echocardiogram treadmill exercise tests, running pharmacological stress tests, performing education with patients about upcoming procedures, helping patients with any questions or concerns that they may have, and helping our assigned doctors.
What’s the biggest change you’ve seen since the COVID-19 outbreak?
CT: The biggest change at work is that hardly anyone is doing much of their normal jobs. All efforts have been focused on combating COVID-19.
MK: The biggest change I have seen since the COVID 19 pandemic is the way Sound practices treatment. We now use video and phone encounters/sessions instead of face to face treatment. When I talk to my clients, most of them enjoy talking by phone, some like the video interactions. Some clients miss coming to the clinic. As a result of sheltering in place, I have noticed more clients make it to their appointments and on time! Most clients worry about the coronavirus and wonder when it will be back to “normal”.
All my encounters are phone/ video at home except once a week I go to the clinic and interact with colleagues and some of the clients who come in for medication management. Upon entering clinic temperatures are taken and all people are to wear masks. Waiting areas and offices are cleaned frequently throughout the day.
BS: The biggest change I have seen since the outbreak is how not only our clinic but the healthcare system as a whole has had to adapt to both protect ourselves and our patients we serve. Currently, our doctors are not seeing any patients in the clinic, unless it is deemed necessary. However, we continue to place heart monitors in the clinic along with running some of our stress tests. We have switched over to virtual visits using Zoom or telephonic visits.
How does an average day for you go?
CT: On an average day, I layer up under my scrubs (because it’s cold in the tent and because I take my scrubs off in the driveway when I come home and put them in a bag before I come into the house). Then, I arrive at the tent. I meet my medical assistant for the day ( it’s always someone new because we are all volunteering wherever they need us). We put on our PPE (personal protective equipment). The PPE consists of a bonnet to cover our hair, a face shield, a mask, a gown, gloves, and shoe covers. We go to the tent and see patients all day who have coughs, fevers, sore throats, or trouble breathing. I decide who should be tested for COVID. The others get treated for colds or strep throat, etc.
MK: My average day starts at 8 in the morning. I phone sessions with clients every 20 minutes for medication management appointments. 60-minute appointments with new clients. I order medications and electronically send medication refills to pharmacies. I have 30 minutes at noon to call colleagues and eat lunch. Then back to calling clients until 4 or 4:30 PM.
BS: I work 4 – 10 hour shifts from 7:00-5:30. From 7:00-8:00 I take temporal temperatures of all employees in the clinic. Masks are handed out at this time as we are required to wear them at work due to COVID-19. At 8:15 we huddle and discuss assignments for the day, which doctors are in the clinic, and any updates that need to be discussed. The remainder of the day we work on our assigned tasks.
What would people not know about how you work?
 CT: I think people don’t know about little things like how cold it is in the tent or that every time we have to go to the bathroom, we have to take all of our PPE off and put all new stuff back on.
CT: I think people don’t know about little things like how cold it is in the tent or that every time we have to go to the bathroom, we have to take all of our PPE off and put all new stuff back on.
MK: Decision making can be incredibly difficult if I don’t have enough data or adequate information because I can’t see my patients in person.
BS: Part of being a nurse is that we not only treat the physical aspect of a patient but the emotional and spiritual aspects as well. Many patients will go into detail about their lives and since we see these patients regularly you begin to know them on a deeper level than just a surface level.
Have you treated any COVID-19 patients? If so, how many?
CT: I do not know exactly how many COVID-19 patients I have treated because I see them before they get tested. I do check on the sick people to make sure that they got their tests. So far, I know there have been for sure nine at the least.
MK: I haven’t treated any COVID-19 patients but I have had clients who have had family or friends die from it so I hear their stories and how they feel.
BS: No, I have not had to treat any COVID-19 patients. However other nurses who currently work in the Cardiac ICU have treated many COVID-19 positive patients.
What’s the hardest part about working since the COVID-19 outbreak?
 CT: There are a lot of hard things about working during COVID-19. From a staffing standpoint, I had to watch a lot of my coworkers get laid off because they weren’t considered essential right now. From a professional standpoint, it is hard and scary to see how sick people are from COVID19. Some of them actually dying. From a personal standpoint, I’m super worried about bringing it home to my kids. I love my job and want to do what I’m doing, but it is scary.
CT: There are a lot of hard things about working during COVID-19. From a staffing standpoint, I had to watch a lot of my coworkers get laid off because they weren’t considered essential right now. From a professional standpoint, it is hard and scary to see how sick people are from COVID19. Some of them actually dying. From a personal standpoint, I’m super worried about bringing it home to my kids. I love my job and want to do what I’m doing, but it is scary.
MK: The hardest part about working since COVID-19 is not seeing clients and colleagues face to face. It’s important in the field of mental health to be able to see people’s faces and the way they respond to you and their environment. It is more difficult with the new clients that I haven’t met in person yet to see their reactions and how they are responding.
BS: The hardest part of working since the COVID-19 outbreak is the unknown. Since a few patients are still coming into the clinic we have had a few exposure scares where multiple people in our office have had to go get tested because a patient subsequently ended up being positive for COVID-19.
What’s something that keeps you going while working?
CT: I am motivated by the fact that this is exactly the reason I decided to go into healthcare. I wanted to make a difference in people’s lives. Hopefully, I am helping at least a little to stop the spread of COVID and to take care of people who get it. Also, community support has been amazing. Free Starbucks, yay!
MK: My clients keep me going while working. They have been more understanding and sensitive. Usually, they don’t ask me how I’m doing but most are at this time. My colleagues have noticed this change, too.
BS: My coworkers definitely keep me going while I am work. We always find ways of joking or making the mood lighter if we are all feeling a bit down. Along with coffee, coffee is amazing!